Advancements in Screening and Treatment Shows Promise
- A new study published in JAMA found that since 1975, the breast cancer mortality rate dropped 58% thanks to improved early detection screenings and treatment for patients in later stages of the disease.
- The Centers for Disease Control and Prevention (CDC) says the overall 5-year survival rate for breast cancer is 90%. However, the survival rate drops sharply for patients in advanced stages; hence, more work still needs to be done.
- The U.S. Preventive Services Task Force recommends women at average breast cancer risk begin screening for breast cancer at age 40. Women with the BRCA gene mutation, who have a family history of cancer or have dense breasts, are at higher risk and should talk with their doctor about when to screen may be younger than 40.
- While mammograms are extremely valuable for breast cancer screening, more effective screening methods exist for women with dense breasts where fatty tissue is harder to see through on imaging scans.
- 3D mammograms, breast ultrasound, breast MRI, and molecular breast imaging are options for women with dense breasts for a more precise screening. It is important to ask your doctor about your breast density and cancer risk.
- The U.S. Food and Drug Administration requires facilities that provide mammograms to tell patients about the density of their breasts. This policy change can directly impact women at higher risk for breast cancer.
- Breast cancer patients who are metastatic, meaning the cancer has spread to distant parts of the body, have more treatment options today to improve their overall quality of life. Food and Drug Administration (FDA) approved drugs like Trodelvy (drug name sacituzumab govitecan) show promise for these patients.
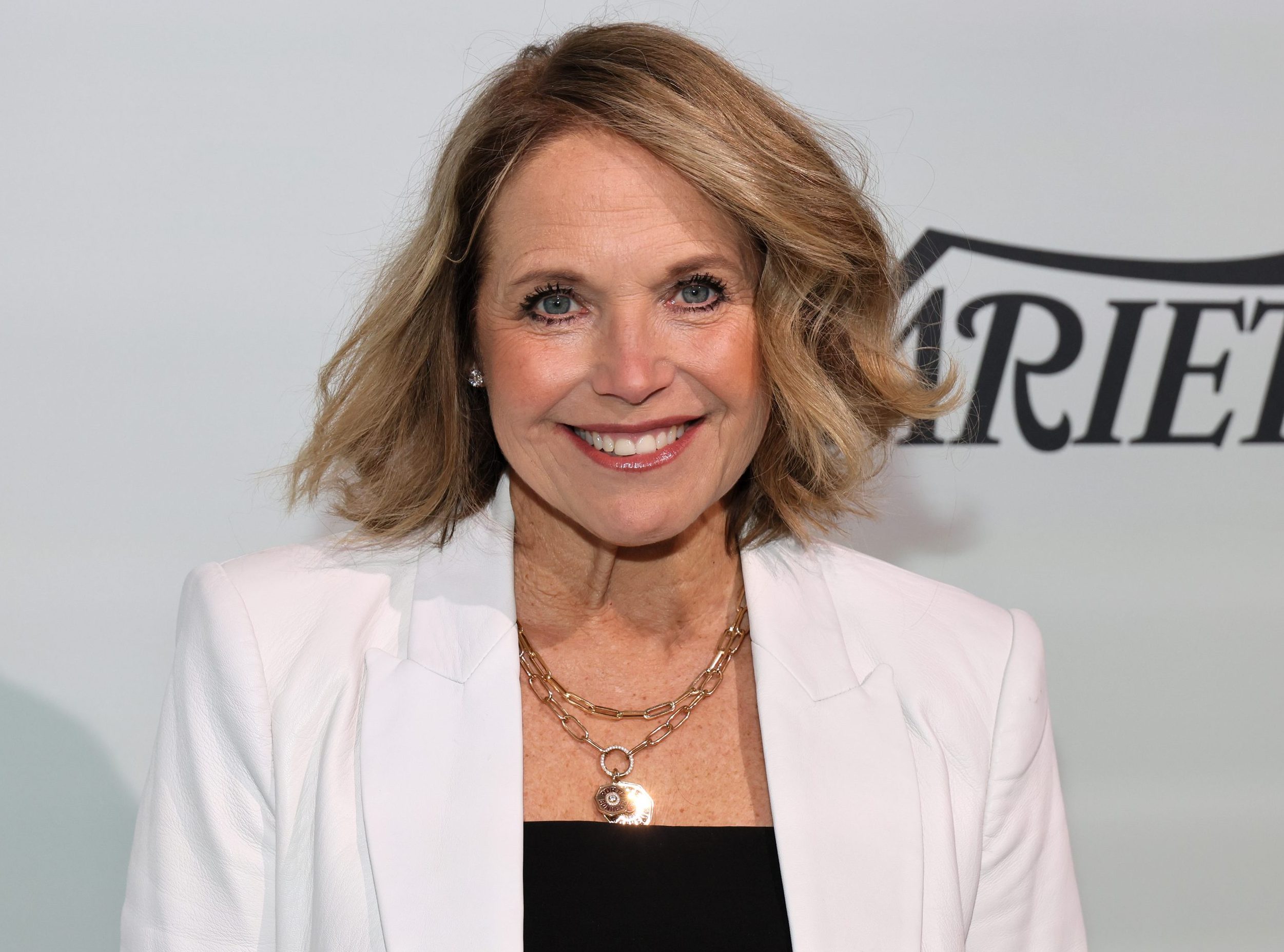
When veteran journalist Katie Couric, 67, was diagnosed with breast cancer two years ago, she used her journey to advocate early detection and breast cancer screenings. Efforts to educate more women to screen for cancer appear to be paying off, according to a new study published in the medical journal JAMA. Researchers say improvements in screening and treatment are associated with a “58% reduction in breast cancer mortality” for breast cancer.
Although the trajectory is moving in a positive direction, more work needs to be done to continue reducing mortality in breast cancer.
Breast cancer mortality varied depending on whether the cancer was estrogen-fueled (ER-positive or negative, HER2 positive or negative).
According to the Centers for Disease Control and Prevention (CDC), the overall 5-year survival rate for breast cancer is 90%. When the cancer remains localized, the survival rate is 98%. When breast cancer is regionalized within the body, the survival rate is 86%. When the cancer has spread to distant parts of the body – metastatic cancer – the survival rate is much lower at only 32%.
The CDC adds that survival is higher when breast cancer is detected in its early stages when it is easier to treat. “Among females diagnosed with breast cancer from 2015 to 2019, 1,097,918 were still alive on January 1, 2020.”
Expert Resources on Breast Cancer Screening
- 30% of Women Say They Have Delayed Mammograms Due to COVID-19, 45% Tell SurvivorNet They're Now More Nervous About Going to the Doctor
- Earlier Mammograms for Black Women May Reduce Breast Cancer Mortality Disparity Rates By 57%; How to Screen for this Disease
- Free Mammograms And Increased Access To Cancer Screenings Focus Of New Bills Promoting Early Detection
- I Have Dense Breasts. Do I Need a 3D Mammogram?
- Inaccurate Mammograms Miss Breast Cancer in 18 Women At Virginia Center: Guidance For Safe Screening
Helpful Information About Breast Cancer Screening
The medical community has a consensus that women between 45 and 54 have annual mammograms. However, an independent panel of experts called the U.S. Preventive Services Task Force (USPSTF) is saying that women should start getting mammograms every other year at the age of 40, suggesting that this lowered the age for breast cancer screening could save 19% more lives. For women aged 55 and older, the American Cancer Society recommends getting a mammogram every other year. However, women in this age group who want added reassurance can still get annual mammograms.
Women with a strong family history of breast cancer, have dense breasts, have a genetic mutation known to increase the risk of breast cancer, such as a BRCA gene mutation, or a medical history, including chest radiation therapy before age 30, are considered at higher risk for breast cancer.
WATCH: Understanding the BRCA gene mutation
Experiencing menstruation at an early age (before 12) or having dense breasts can also put you into a high-risk category. If you are at a higher risk for developing breast cancer, you should begin screening earlier.
Breast density is determined through mammograms. However, women with dense breasts are at a higher risk for developing breast cancer because dense breast tissue can mask potential cancer during screening. 3D mammograms, breast ultrasound, breast MRI, and molecular breast imaging are options for women with dense breasts for a more precise screening. It is important to ask your doctor about your breast density and cancer risk.
Family History & Breast Cancer Risk
Although breast cancer can happen to anyone, certain factors can increase a person’s risk of getting the disease. The known risk factors for breast cancer include:
- Older age
- Having a gene mutation such as the BRCA1 or BRCA2
- Added exposure to estrogen
- Having children after the age of 30
- Exposure to radiation early in life
- Family history of the disease
RELATED: Is Genetic Testing Right for You?
Different types of genetic testing can help people with a family history of cancer better ascertain their cancer risks. Your doctor will discuss your family history of cancer with you in the context of your type of tumor and your age at diagnosis. Hereditary genetic testing is usually done with a blood or saliva test.
WATCH: Understanding genetic testing for breast cancer.
About ten percent of breast cancers are hereditary, says Dr. Ophira Ginsburg, Director of the High-Risk Cancer Program at NYU Langone’s Perlmutter Cancer Center.
“We encourage only those with a family history to get [genetic testing],” Dr. Ginsburg tells Survivornet.
“I would say that if you have anyone in your family diagnosed with a rare cancer. Or if you have a strong family history of one or two kinds of cancer, particularly breast and ovarian, but also colon, rectal, uterine, and ovarian cancer, that goes together in another cancer syndrome called the Lynch Syndrome,” Dr. Ginsburg adds.
The second test involves the genetic sequencing of your tumor if you’ve been diagnosed with cancer by this point. These genetic changes can be inherited, but most arise during a person’s lifetime. This process usually involves examining a biopsy or surgical specimen of your tumor. This testing can lead to decisions on drugs that might work against your cancer.
“Digital mammography, it turns out, significantly improves the quality of the mammogram… It’s 3D or tomosynthesis mammography,” Dr. Lehman explains.
“This allows us to find more cancers and significantly reduce our false-positive rate. With digital mammography 3D tomosynthesis, we’re taking thin slices through that breast tissue, like slices of a loaf of bread. We can look at each slice independently rather than trying to see through the entire thickness of the entire loaf of bread. So those thin slices help us find things that were hidden in all the multiple layers,” Dr. Lehman adds.
Additional testing can be considered for dense breasts, depending on a woman’s personal history, preferences, and her physician’s guidance.
Screening Options for Women with Dense Breasts
Women with dense breasts should get additional screening to supplement their mammograms. Dense breasts mean more fibro glandular tissue and less fatty breast tissue exists.
The dense tissue has a “masking effect on how well we can perceive cancer and find cancer on mammograms,” Dr. Cindy Ly, a radiology doctor at NYU Langone Medical Center, told SurvivorNet.
WATCH: Understanding dense breast mammography
Glandular tissue within dense breasts appears white on mammograms, which can help mask potential cancer. The “frosted glass” effect from the glandular tissue can thus mask cancerous areas, especially developing ones. Undetected, these cancers can progress, growing large and advanced. They will then likely require more intensive treatments to cure or can become incurable altogether.
Advancements in Breast Cancer Treatment
If you are diagnosed with late-stage breast cancer, you should know you still have many treatment options to improve your quality of life. For metastatic breast cancer patients, the drug Trodelvy (drug name sacituzumab govitecan`) is showing promise. Metastatic or stage 4 cancer means the cancer has spread to distant parts of the body.
Trodelvy is a type of drug called an antibody-drug conjugate, which is an antibody and drug combined. It works because the anti-cancer drug is attached to an antibody that recognizes cancer cells. When the drug enters the bloodstream, the antibodies deliver the anti-cancer drug directly to the cancer cells by IV infusion. Since the drug goes straight to cancer cells, it has minimal effects on healthy cells.
WATCH: How Trodelvy Offers Hope
Traditional chemotherapy, on the other hand, doesn’t target cancer cells as strictly. It can damage healthy cells, too. That’s what causes the side effects for which chemo is well known.
That doesn’t mean that Trodelvy is without side effects. Roughly one in ten people who take the drug have severe diarrhea, and roughly half hit very low levels of the type of white blood cell (neutrophils) that help fight bacterial infections.
Recent results from a trial show the phase III TROPiCS-02 study presented at the European Society for Medical Oncology (ESMO) Congress 2022 showed that Gilead’s drug, Trodelvy, demonstrated exciting results for breast cancer patients who had hormone-sensitive tumors that tested negative for a receptor called HER2 and who had stopped responding to at least two earlier courses of therapy.
Hormone-positive (HR+) and HER2-negative (HER2-) breast cancer is the most common type of breast cancer, accounting for about 70% of new cases worldwide per year. HER2 stands for human epidermal growth factor receptor 2. It’s a protein that helps breast cancer cells grow quickly. The presence of HER2 has been divided into two groups, either positive or negative, leaving about 50 percent of patients somewhere in the middle. These groupings are based on how the tumors appear under a microscope when graded by the pathologist or with additional testing a pathologist may perform.
Patients with HER2-positive tumors have tumors that show HER2 over-expression, while patients with HER2-negative tumors show minimal or no expression.
Phase III trials represent one of the highest levels of scientific evidence available in medicine.
The study presented at the ESMO’s annual meeting in Paris compared Trodelvy to chemotherapy in 543 patients. Trodelvy extended by 3.2 months the survival of patients with advanced stages of a common type of breast cancer. Put another way, the Gilead drug reduced the risk of death by 21%.
“This is very encouraging data for women whose cancers are hormone receptor-positive. So yes, it’s very, very exciting. I don’t think we can actually start using the drug in the clinic until we have approval. That may be forthcoming, we hope it is,” Dr. Ruth Oratz, a medical oncologist at NYU Langone Perlmutter Cancer Center in New York City, told SurvivorNet.
Last year, the U.S. Food and Drug Administration (FDA) approved the drug called alpelisib (also known by its brand name, Piqray), which could help metastatic breast cancer patients.
“Now our patients will have one more non-chemo option,” Dr. Jame Abraham, Director of Breast Oncology at Cleveland Clinic, told SurvivorNet. “Most importantly, it is a first-in-class drug, which showed significant improvement in progression-free survival.”
As a “first-in-class drug,” Piqray is the very first PI3K inhibitor to enter the market for breast cancer treatment. A PI3K inhibitor is a drug that works by blocking the PI3K (phosphoinositide 3-kinase) enzyme, which has an essential function in allowing cells, including cancer cells, to grow.
For breast cancer patients diagnosed with triple-negative breast cancer – an aggressive form of the disease – Trodelvy (sacituzumab govitecan) significantly prolonged life and progression-free survival. It’s called triple-negative because it does not have any of the main drivers of breast cancer, the estrogen receptor, the progesterone receptor, and the HER2 receptor, and doesn’t respond to the currently available treatments that target them. However, experts tell SurvivorNet that the disease often responds well to chemotherapy.
WATCH: Understanding triple-negative breast cancer.
The FDA approved Trodelvy for the treatment of metastatic triple-negative breast cancer in women who had already received two previous types of treatment. Trodelvy works by attaching the anti-cancer drug to an antibody that recognizes cancer cells and then kills it directly with minimal effects on healthy cells, reducing side effects.
The new data released last week, based on 468 patients, show that women who take Trodelvy survive a median of 12.1 months compared to those who survive a median of 6.7 months on chemotherapy. The drug halted disease progression for a median of 5.6 months, compared to 1.7 months on chemotherapy.
Couric’s Courageous Cancer Journey
Couric was diagnosed in June 2022 but revealed her cancer to the world during Breast Cancer Awareness Month last year. She said in an essay for Katie Couric Media that her diagnosis came on her wedding anniversary. She added before her diagnosis, she hadn’t had a mammogram since December 2020, so she was long overdue.
“You’re due for a mammogram,’ my gynecologist said, looking over my medical chart. It was May; I had just gotten a pap smear and was still sitting on the exam table in my pink cotton (open in the front) gown,” Couric wrote. “‘That’s crazy, I just got one!’ I told her, with a hint of indignation.”

After receiving a 3D mammogram, a breast ultrasound, and a biopsy, Couric was diagnosed with stage 1A, hormone receptor-positive, Her2-negative breast cancer. She’s since undergone a lumpectomy and radiation treatment, but she’ll need to take an aromatase inhibitor for five years.
“I was nervous about it. I waited a few days so I could process it and really understand what we were dealing with,” Couric said to “Today” at the time.
Dr. Michael Zeidman, assistant professor of surgery at Icahn School of Medicine at Mount Sinai in New York City, tells SurvivorNet that stage 1 is divided into two subcategories, 1a and 1b. Stage 1a breast cancer means the cancer hasn’t spread outside the breast. Stage 1b means there’s no tumor in the breast; instead, small groups of cancer cells are found in the lymph nodes. Stage 1b can also mean there’s a tumor in the breast and small groups of cancer cells in the lymph nodes. Stage 1 also means the cancer was caught very early, he says.
She underwent surgery and radiation therapy to treat the cancer a few months after her diagnosis.
Her lumpectomy was performed in a process called wireless localization, which makes it easier for surgeons to locate tumors and less uncomfortable for the patient. It replaces the traditional wire placement patients must get before lumpectomy surgery.
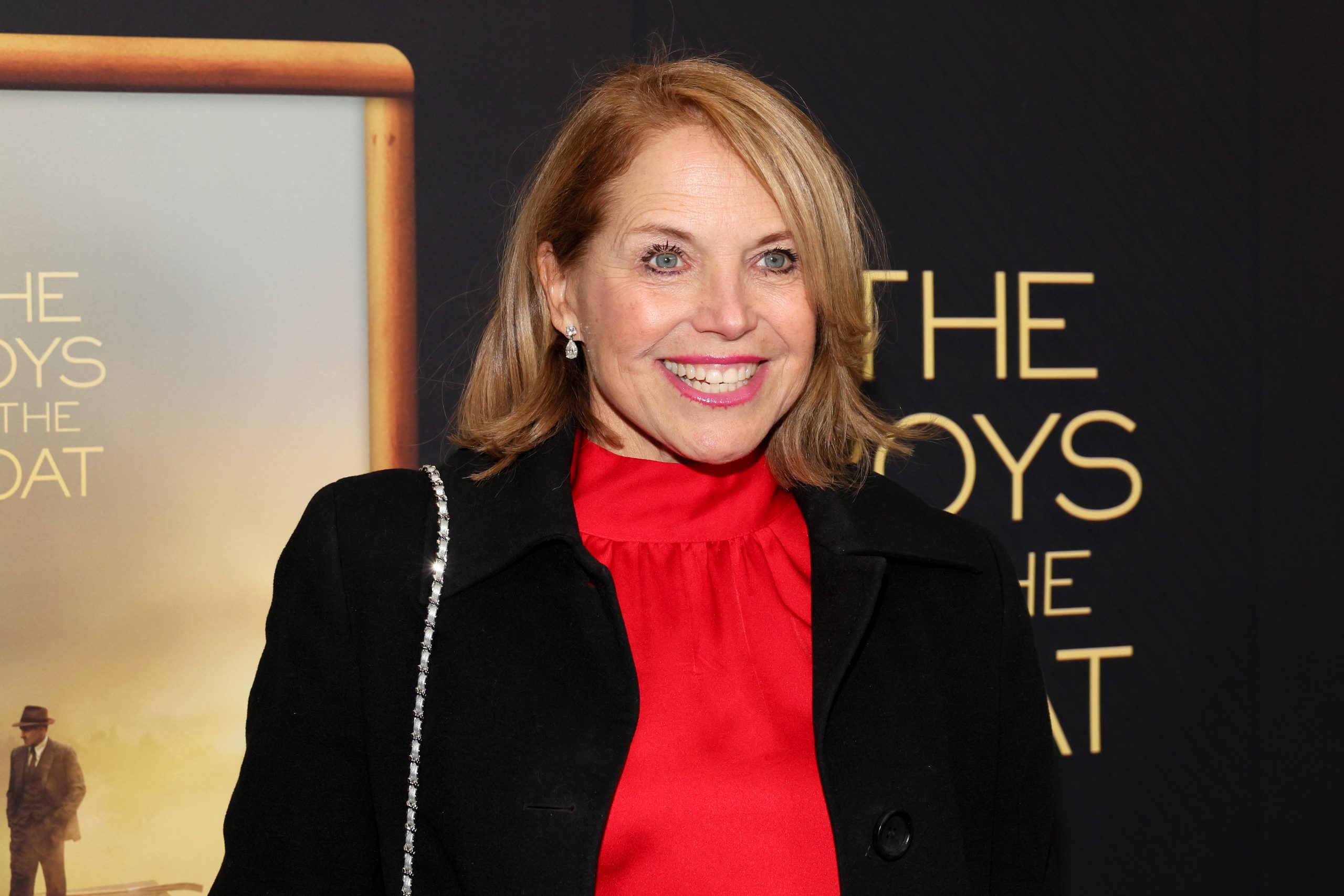
This new technique functions much like a GPS in your car or phone and involves the insertion of a small tag or device onto your tumor several days before surgery. Then, on the day of surgery, the surgeon can locate the device and remove the tumor.
Perhaps equally as important is she learned more about her breast during her cancer journey. She has dense breasts, meaning more fibroglandular tissue and less fatty breast tissue exist.
Couric says she receives additional screening alongside her mammogram. She also receives an ultrasound. A breast ultrasound can supplement a regular mammogram in women with dense breasts.
Couric has used her public platform to advocate cancer awareness and promote healthy living. Following the emotional passing of “Jeopardy” game show host Alex Trebek, Couric partnered with Alex’s widow, Jean, to launch the “Alex Trebek Fund,” created to help support research into pancreatic cancer.
Questions for Your Doctor
If you have a breast cancer screening coming up or recently had one, you may have questions you want answered. SurvivorNet suggests the following questions to kickstart your conversation with your doctor.
- Do my mammogram results indicate I have breast cancer, or am I at higher risk?
- If I’m at higher risk, what are my treatment options?
- What side effects should I expect related to my treatment?
- How much will this diagnosis prevent me from working or fulfilling my daily activities?
- Will insurance cover my breast cancer screening, or are there other financial resources available?
Learn more about SurvivorNet's rigorous medical review process.
